As of 2026, creating a wearable kidney remains a significant challenge because researchers are typically attempting to condense a room-sized dialysis infrastructure into a device small enough to be worn under clothing. While a few models have reached human trials, the following factors continue to delay widespread production:
1. Water Regeneration and Miniaturization
Traditional hemodialysis requires over 100 liters of ultrapure water per session. For a device to be wearable, it must recycle a very small amount of fluid continuously.
- Water Recycling: Developing “smart” filters or sorbent systems that can continuously clean and reuse dialysate without needing an external water source is a major engineering hurdle.
- Weight Challenges: Early prototypes weighed as much as 11 lbs, though the latest WAK 3.0 version has successfully been reduced to 2 lbs.
2. Complex Biological Functions
A human kidney does more than just filter waste; it also regulates blood pressure, produces hormones, and maintains electrolyte balance.
- Homeostasis: Artificial devices must be able to communicate with the body’s environment to keep blood chemistry constant, a multifactorial task that is much harder than replicating a single-function organ like the heart.
- Biocompatibility: Keeping blood from clotting when it touches synthetic filters (thrombogenicity) remains a constant risk, often requiring patients to use blood thinners, which is not ideal for long-term wearable use.
3. Technical Malfunctions in Trials
Clinical trials have frequently been halted due to “real-world” technical issues that occur when a device is mobile:
- Gas Bubbles: Excessive carbon dioxide bubbles in the fluid circuit have stopped previous human trials.
- Hardware Failure: Issues such as tubing kinks, fluctuating pump speeds, and battery reliability are critical safety risks that must be perfected before a device can be cleared for home use.
4. Funding and Manufacturing Gaps
Despite the high demand, research into kidney innovation receives relatively modest funding compared to other medical fields.
- Funding Shortfalls: Prominent projects like The Kidney Project estimate they need at least $10 million in additional funding just to complete the preclinical work required for human trials.
- Industry Hesitation: Large dialysis manufacturers have shown little motivation to develop smaller, portable kidneys, forcing smaller research teams to take the lead. Many existing medical manufacturers also lack experience with the specialized silicon technology needed for these miniaturized filters.
Current Status (2026)
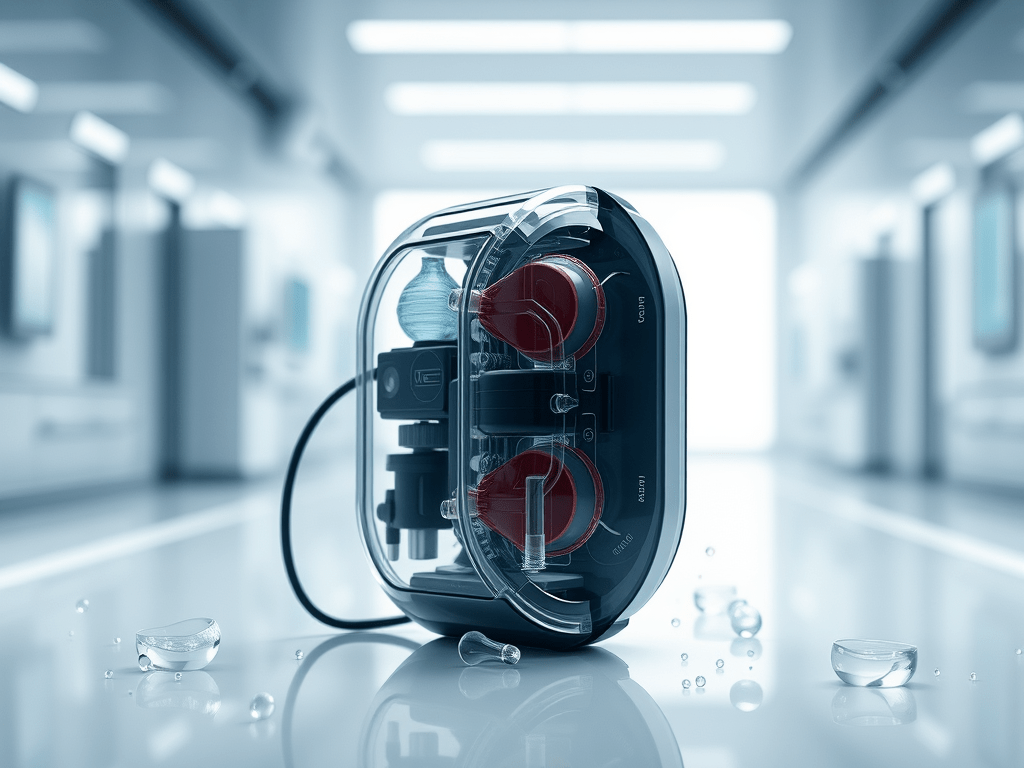
- The WAK 3.0: This 2-pound device has completed three human trials and has two more study phases to complete before it can be released to the public.
- The Neokidney: A “luggage-sized” portable machine (larger than wearable) recently began clinical trials in early 2026.
- The Bioartificial Kidney: An implantable version is roughly 2–3 years away from starting clinical trials.
However, miniaturization of current dialysis machines is not the only path to a wearable or artificial kidney. While several projects focus on downsizing hemodialysis (HD) and peritoneal dialysis (PD) equipment, other fundamentally different technologies are being developed.
1. Miniaturized Dialysis Systems
These technologies adapt existing dialysis principles into portable or wearable formats by reducing the need for large quantities of water.
- Wearable Hemodialysis (WAK): A belt-sized device (approx. 5 kg) that uses a closed-loop system to continuously regenerate a small amount of dialysate (under 500 cc).
- Wearable Peritoneal Dialysis (AWAK/VIVANCE): These systems, such as the VIVANCE (formerly AWAK), use sorbent technology to continuously purify and recycle dialysis fluid from the peritoneal cavity, fitting into a shoulder bag.
2. Bioartificial and Hybrid Technologies
These approaches move beyond traditional mechanical filtration by incorporating biological components or advanced nanotechnology.
- Implantable Bioartificial Kidney: Projects like “The Kidney Project” (UCSF/Vanderbilt) use a silicon membrane filter for mechanical waste removal combined with a bioreactor containing engineered human kidney cells to handle electrolyte balance and metabolic functions.
- Nanofabrication: Instead of traditional fiber filters, researchers are using semiconductor technology to create silicon nanopore membranes. These allow for high-efficiency filtration driven solely by a patient’s own blood pressure, potentially eliminating the need for bulky electrical pumps and batteries.
3. Alternative Regenerative Paths
Other scientific avenues aim to replace kidney function entirely rather than mimicking it with a machine.
- Xenotransplantation: This involves transplanting kidneys from genetically engineered pigs. Breakthroughs in 2025 and 2026 have explored using pigs with multiple genetic modifications to prevent immediate rejection by the human immune system.
- Regenerative Medicine & 3D Bioprinting: Scientists are working on 3D printing kidney tissue or growing “organoids” from stem cells. While these are currently limited to modeling disease or maturing to second-trimester fetal stages, the long-term goal is to grow functional replacement organs.
- Kidney-on-a-Chip: Advanced microfluidic platforms are being used to replicate human glomerular and tubular functions for drug testing and as a potential precursor to more complex bioartificial devices.



Leave a comment